Call us on 07340 388567
Click on a condition to find out more about what we do
Joint Hypermobility
Movement Disorders
Toe Walking
Postural Difficulties
Muscular Dystrophies
Balance Difficulties
Cerebral Palsy
Plagiocephaly
(Flat Head Syndrome)
Coordination Difficulties
Developmental Delay
Syndromes
Torticollis
Flat Feet
Unknown
Joint Hypermobility
What is Hypermobility?
Joint hypermobility is what some people refer to as having "loose joints" or being "double-jointed”. Joint hypermobility means that some or all of a person's joints have an unusually large range of movement. People with hypermobility are particularly supple and able to move their limbs into positions others find impossible. It may be present in just a few joints or it may be widespread. It is most common in childhood and adolescence, in females, and Asian and Afro-Caribbean races.
Not all children who are hypermobile have the syndrome. Between 10-50% of all children are hypermobile but far fewer have the associated symptoms related to the syndrome.
Symptoms?
Many people with hypermobile joints don't have any problems, and some people – such as ballet dancers, gymnasts and musicians – may actually benefit from the increased flexibility.
However, some people with joint hypermobility can have a number of unpleasant symptoms as well, such as:
- pain and stiffness in the joints and muscles
- fatigue (extreme tiredness)
- abdominal pain (includes digestive problems such as constipation, irritable bowel syndrome and cow’s milk protein allergy)
- headaches
- clicking joints
- joints that dislocate (come out of the correct position) easily
- recurrent injuries such as sprains
- dizziness and fainting
- thin or stretchy skin
If hypermobility occurs alongside some of these symptoms, it is known as Joint Hypermobility Syndrome (JHS). This has to be assesed and diagnosed by a Paediatrician.
The musculoskeletal symptoms are related to the strength and fitness of the muscles and not the amount of extra movement the joint has. The less strength and fitness a muscle has the greater the pain experienced. The pain is often most prominent after activity, at the end of the day and at night and this indicates that the muscles are not strong enough or fit enough for the whole day and all the activities. More rest will only increase the symptoms. In general the muscles of children with JHS get weaker quicker than average and take longer to regain strength and so any activity that reduces mobility and activity will in fact make the symptoms ultimately worse.
Causes?
Joint hypermobility often runs in families. One of the main causes is thought to be genetically determined changes to a type of protein called collagen. Collagen is found throughout the body e.g. in skin and ligaments. If collagen is weaker than it should be, tissues in the body will be fragile, which can make ligaments and joints loose and stretchy. As a result, the joints can extend further than usual.
Joint Hypermobility Syndrome is widely thought to be a feature of an underlying condition affecting connective tissue called Ehlers-Danlos syndrome (EDS).
Living with joint hypermobility
Most people with hypermobile joints won't experience any problems and won't require any medical treatment or support. However, Joint Hypermobility Syndrome can be very difficult to live with because it can cause such a wide range of symptoms.
People with Joint Hypermobility Syndrome often benefit from a combination of controlled exercise and Physiotherapy, as well as additional help to manage pain and make everyday tasks easier.
The nature of Joint Hypermobility Syndrome means that you are at increased risk of injuries, such as dislocations and sprains. Managing the condition may therefore also involve treating short-term injuries as they arise, while following a long-term treatment plan to manage daily symptoms.
Treatment
Effective management of the symptoms of JHS is very possible nowadays.
The evidence shows that pain medication is not effective in managing the pain and fatigue and can in fact make other symptoms, such as abdominal pain, constipation and head ache worse.
The most effective management for this condition is a combination of physical and psychological techniques.
Physiotherapy will focus on a progressive resisted specific exercise programme. This approach is designed to ensure that each muscle is strengthened so that the joints are protected and the hypermobile range used effectively in order to reduce pain and fatigue and to ensure the body is fit enough so that complex activities such as sport and physical activities can be completed safely.
In some cases an Occupational Therapy referral will be made to focus on handwriting skills, pacing skills and advice for schools.
With the correct approach this condition can be well managed and young people are able to participate fully in school and other activities with relatively well-controlled pain and fatigue.
At Children in Motion we understand that each child will need a tailor made progressive resisted specific exercise programme that empowers and helps them to make a positive change. We will also assess whether your child has any other related problems such as flat feet, shoulder or hip problems and asymmetries such as in the spine.
Movement Disorders

Movement disorders affect the way a child’s body moves. These conditions can include too much or too little movement, or co-ordination problems. Movement disorders may be caused by injuries to the brain, genetic or metabolic conditions, medications, inflammatory or autoimmune disorders, or post infections.
One of the most common movement disorders, Cerebral Palsy, is described on it's own page. Movement disorders are complex and cover a vast amount of varying conditions. If your child has been diagnosed with a movement disorder or if you have concerns that your child might be affected by a movement disorder, please contact us to see if we could be of assistance.
Toe Walking
Many children walk on tip toes and this can be a normal part of their development. It is more common in boys and it can sometimes be seen in several family members.
Walking on tip toes generally does not cause the child any pain or discomfort and it does not result in any type of deformity. However it may lead to tightening of the calf muscle and shortening of the Achilles tendon which can lead to the child being unable to put their heel to the ground and cause difficulties with balance and more frequent falls.
Seek advice when your child:
- Walks on their toes most of the time
- Has stiff muscles
- Is uncoordinated
- Walks awkwardly, stumbles, or has a waddling gait
- Has fine motor skills that don't seem to be developing normally (for example, they can't button their shirt)
- Seems as though they can't bear their weight on a flat foot
- Loses motor skills that they already had, i.e. finding it difficult to stand up from sitting down on the floor
Causes?
If your child has always tiptoed, it's possible that they have a physical problem, such as a short Achilles tendon (tendon behind the heel), that actually prevents them from standing flat-footed and limits their range of motion in the ankle.
If their muscle tone is fine, and they have a good range of motion in the ankle – then they'll likely be diagnosed with what's called idiopathic toe walking (i.e. the cause is unknown).
Consistent toe walking is more likely a sign of a motor disorder – most commonly, a form of cerebral palsy.
In some rare cases there may be an underlying muscle problem.
Treatment?
Stretching, insoles, botox, casting, surgery
Physiotherapy - Treatment will depend on the age of the child and whether there is tendon shortening or an underlying problem. The child and family will be shown muscle stretching exercises that need to be practiced at home every day, along with activities to encourage feet flat on the floor. Advice will be given about recommended footwear to help maintain a good foot position.
Orthotics - your child may be referred for insoles or ankle foot orthoses (foot splints)
Serial Casting - is sometimes used. In this procedure, a series of casts stretch and lengthen the tendon and increase the range of ankle movement.
In rare cases when casting does not help, or if the toe-walking starts again after a time, the child may need special injections (Botulinum Toxin injections) into the tight muscles.
In some cases, surgery will be recommended.
At Children in Motion we feel it is important to look at the child holistically and not just at the ankle and calf muscle in isolation. We therefore do a thorough assessment of the whole body’s joints and a functional movement analyses to ensure there aren’t any underlying causes or knock-on effect on their musculoskeletal system that needs addressing.
Postural Difficulties
Posture is the manner and position in which your child holds his head, neck, back and spine, as well as his arms and legs, when standing, sitting or lying down.
Children are spending extended time in static postures whilst using technology, such as tablets, computer games, television, this is having an impact on their developing postures.
The effect of a poor posture can vary from back and head ache to more severe implications such as spinal curvatures including kyphosis and scoliosis. Sometimes PROBLEMS CAN be solved with simple advice such as CHANGING THE seating set-up at a desk when studying or working on a computer; carrying bags on back; or small changes such as sitting on a stability ball when playing computer games.
Treatment?
Physiotherapy is essential in both advising on better posture as well as muscle strengthening and postural training in improving awareness of what a good posture is. If your child has already developed a scoliosis and/or kyphosis it will require a more intense treatment programme over an extended period of time.
Muscular Dystrophies
What is Muscular Dystrophy?
Muscular dystrophies are a group of inherited genetic conditions that gradually causes muscles to weaken. This leads to an increasing level of disability. Muscular Dystrophy is a progressive condition, which means that it gets worse over time. It often begins by affecting a particular group of muscles before becoming more widely spread. Some types of Muscular Dystrophies also affect the breathing muscles and heart. There is no cure for Muscular Dystrophy, but treatment can help manage many of the symptoms.
Causes?
Muscular Dystrophy is caused by changes in the genes responsible for the structure and functioning of a person's muscles and is often inherited from a person’s parents. These mutations cause changes in the muscle fibres that interfere with the muscles' ability to function. Over time, this causes increasing disability.
Types of Muscular Dystrophy?
There are many different types of Muscular Dystrophy, each with somewhat different symptoms. Not all types of Muscular Dystrophy cause severe disability and some do not affect life expectancy.
One of the most commonly known and severe forms of Muscular Dystrophy is Duchenne Muscular Dystrophy. It mainly affects boys in early childhood. It affects around one boy in every 3500 in the United Kingdom.
Treatment?
There is currently no cure for Muscular Dystrophy, but a variety of treatments can help to manage the condition and optimise physical ability, including:
- Physiotherapy – can be useful for maintaining muscle strength, preserving flexibility and preventing stiff joints. Your Physiotherapist will help you with physical aids, such as a wheelchair, leg braces or crutches that can help you maintain standing and stay mobile for as long as possible. When the breathing muscles start to weaken your Physiotherapist will also be able to advise you on chest physiotherapy and respiratory management using machines.
- Breathing assistance - Once the chest muscles become too weak to control breathing properly, you may require machines to assist with your breathing and coughing, especially while sleeping.
- Medication – there are a variety of medications which can help with treating symptoms.
- Surgery – In some severe cases of Muscular Dystrophy, surgery may be necessary to correct physical problems that can occur as a result of the condition such as scoliosis and to release tight muscles.
At Children in Motion it will be our aim to support your child alongside their NHS team to ensure their therapy input is coordinated and consistent
Balance Difficulties
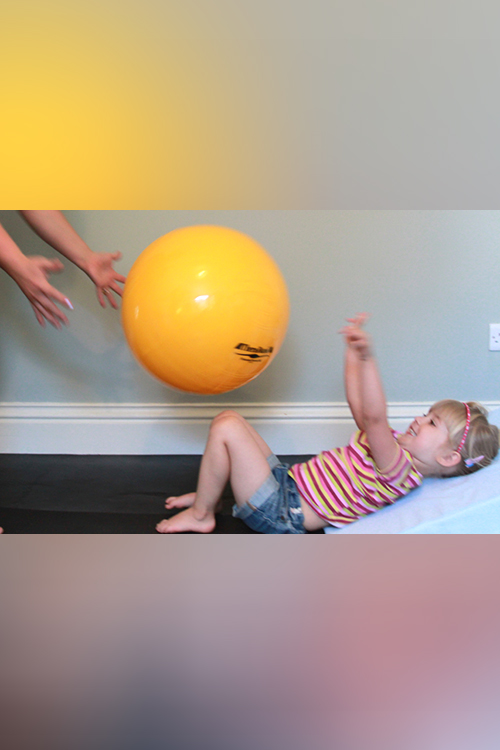
The cause of balance difficulties in children can vary widely. It could be due to problems with your child’s ears. It could go hand in hand with coordination difficulties and that your child is generally clumsy (please see coordination difficulties for more information). It could also be due to neurological conditions such as cerebral palsy (please see cerebral palsy for more information).
Physiotherapy will be tailored depending on the cause of your child’s balance difficulties.
At Children in Motion we will complete an in-depth assessment to determine the cause of your child’s balance difficulties. Then treat accordingly or refer your child to the appropriate medical team for further investigations.
Cerebral Palsy
What is Cerebral Palsy?
“Cerebral palsy describes a group of permanent disorders of the development of movement and posture, causing activity limitation, that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain. The motor disorders of CP are often accompanied by disturbances of sensation, perception, cognition, communication, behaviour, by epilepsy and by secondary musculoskeletal problems.”(Modified after Bax et al. 2005)
Cerebral Palsy is a very broad term given to disorders of movement and posture. The damage to the brain is in the parts responsible for controlling movement and is permanent but not progressive, but because children are growing, in practice, we see symptoms which appear progressive i.e. children might get tightness in their muscles or develop deformities such as curvatures of their spines which may require surgery. Other parts of the brain responsible for functions such as communication, hearing, vision and the ability to learn may also be affected.
How Many Children are affected?
Approximately 2 children in a 1000 are affected by Cerebral Palsy.
Causes of Cerebral Palsy?
There are many causes of Cerebral Palsy of which the following are a few:
- Before birth
- Damage to the brain’s white matter (Periventricular Leukomalacia) – it is not clear exactly why this occurs, but has been linked to
- Premature birth (especially when the child is born at 32 weeks gestation or earlier)
- Maternal infection
- The mother suffering with abnormally low blood pressure
- Abnormal development of the brain
- Changes in the genes that play a role in the brain’s development
- An infection caught by the mother
- Trauma or injury to the unborn baby’s head
- Bleeding in the brain and Stroke
- Premature birth
- Pre-existing weakness or abnormalities in the baby’s blood vessels or them mother’s placenta
- High blood pressure in the mother
- An infection caught by the mother
- Damage to the brain’s white matter (Periventricular Leukomalacia) – it is not clear exactly why this occurs, but has been linked to
- During birth
- Temporary deprivation of oxygen during a difficult or complicated birth (Asphyxiation)
- After birth
- Infection of the brain such as meningitis
- Serious head injury
- Stroke
- Kernicterus – caused by dangerously high levels of bilirubin (jaundice)
Symptoms?
The common feature of this broad group of children who have Cerebral Palsy is a problem of co-ordination of posture and movement due to a disturbance of postural/muscle tone resulting from brain damage.
Muscle tone is the term used to describe the relative stiffness or floppiness of our muscles. Tone needs to be high enough to keep you up against gravity but low enough to allow you to move. Muscle tone which falls within the normal range provides both stability and mobility for our body which allows for a choice of selective movement patterns and quick adaptation, enabling us to perform skilled activities e.g. standing on a moving train.
The main symptoms largely depend on the specific form of Cerebral Palsy a person has.
The four main types of Cerebral Palsy are:
- If muscle tone is too high, the muscles feel stiff and this is called hypertonia or spasticity. A child with this quantity of tone will feel stiff and we feel resistance to moving a certain part of their body. The child will have difficulty initiating movement and movement is slow. With the effort of moving they often become even stiffer and therefore less able to move.
- If muscle tone is too low, the child will feel floppy and this is called hypotonia. The child lacks activity making it difficult for them to initiate movement against gravity.
- Some children have muscle tone which fluctuates from too low to too high or is very changeable. This is seen in children who have athetosis.
- Balance and co-ordination problems, resulting in jerky and clumsy movements are seen in children with ataxia.
The symptoms of cerebral palsy differ in severity from person to person. Some people will only have mild problems, while others will be severely disabled. The Gross Motor Function Classification (PDF) system has been developed to group children in their functional abilities.
The areas affected by cerebral palsy can also vary. Some people are only affected on one side of the body (hemiplegia), some are affected in the whole body but with the legs more affected (diplegia) and others are affected in the whole body with the arms more or equally affected as the legs (quadriplegia).
The following could also be associated with Cerebral Palsy:
- Epilepsy
- Hydrocephalus
- Constipation
- Visual problems such as squints, cortical blindness, etc
- Hearing
- Sensory difficulties
- Perceptual difficulties
- Eating and drinking difficulties
- Communication difficulties
- Learning difficulties
- Emotional and behavioural difficulties
- Contractures and deformities
Treatment for Cerebral Palsy?
There is no cure for cerebral palsy, but a range of treatments are available to help treat many of the symptoms.
Treatment for cerebral palsy will usually involve a team of health professionals with different areas of expertise. The team may include a Paediatrician, Health Visitor, Portage Worker, Social Worker, Physiotherapist, Orthotist, Speech and Language Therapist, Occupational Therapist, Teacher specialising in helping children with visual impairment, Educational Psychologist.
There are a wide range of treatments available, which are designed to improve your child's symptoms and let them be as independent as possible. Some of the main treatments available are Physiotherapy; Speech and Language Therapy; Occupational Therapy; Hydrotherapy; Drug treatment such as Diazepam, Baclofen, Botulinum Toxin injections; Surgery such as orhtopaedic surgery and selective dorsal rhizotomy (SDR)
At Children in Motion our assesment is holistic, focussing on the quality of movemnet alongside a functional movemnet analysis. Our treatment is based on the Bobath Concept which is explained under Treatment, in combination with other treatment modalities such as strength training, orthotics, treadmill training and kinesiotex taping.
Plagiocephaly (Flat Head Syndrome)
What is Flat head syndrome?
Babies sometimes develop a flattened head when they're a few months old, usually from sleeping on their back. It's known as "flat head syndrome" or "moulding" and there are two types – plagiocephaly (flattening on one side) and brachycephaly (flattening on the back of the head).
Causes?
The skull consists of plates of bone, which start to strengthen and fuse together as a child develops and gets older. A young baby's skull is still soft enough to be moulded and change shape if there's constant pressure on a particular area of their head.
- A baby's sleeping position - The main cause of flat head syndrome is sleeping on their back every night, although there may be other factors at work. Should the back or one side of the baby's head (if their head naturally rolls to the side) be squashed against a firm mattress, the soft bone of their skull can become flattened. Once their head is flattened, it will automatically stay on the flattened side or roll towards it. This will then become their preferred side for sleeping and for resting their head during the day.
Do not change your baby's sleeping position. It's very important for babies to sleep on their back, because it reduces the risk of sudden infant death syndrome (SIDS) or otherwise known as cot death. - Baby equipment such as car seats - today’s prolonged use of car seats and other baby equipment mean that your baby is unable to move freely and is susceptible to head moulding. Try to minimise and use only when your baby is actually in the car and not for longer than 2 hours per day
- Factors in the womb - flattening of a baby's skull can sometimes occur in the mother's womb (moulding), e.g. with reduced amniotic fluid or multiple births where twins squash against each other.
- Premature births - premature babies are more likely to have an altered skull shape because they have been squeezed through the birth canal when their skulls haven't fully developed (the skull strengthens during the last few weeks of pregnancy). Babies born prematurely tend to be nursed with their head on the side (alternately), which means they can develop a longer, thin head (similar shape to scaphocephaly). As these babies are born early, they also have a longer period of time before they develop head control and are able to spontaneously move their heads.
- Muscle problems - a baby will sometimes have tight muscles in their neck, which prevents them from turning their head a particular way (toriticollis). This causes them to always rest their head on the other side, flattening it.
- Craniosynostosis - A flattened head can sometimes be caused by the bony plates of a baby's skull joining together too early. This is known as craniosynostosis. This can pull the baby's head out of shape and may need to be corrected with surgery.
Treatment?
- Physiotherapy – even if your baby has mild flat head syndrome it is always good to seek advice from a Physiotherapist:
- To ensure there are not other related issues such as torticollis
- For advice regarding positioning and activities during day time. At Children in Motion we have published a Tummy Time Poster with activities and positioning which could be a useful reminder. Contact us for a copy.
- To help with potential related gross motor developmental issues
- Cranial Orthotics (Headband or helmet therapy) – this treatment is an option when repositioning techniques have not brought about sufficient improvement in your baby's Plagiocephaly or head shape, but it should not be considered until the infant is at least 4 to 5 months old. It works by applying a gentle constant pressure over the areas of your baby’s skull which are most prominent while allowing unrestricted growth over the flattened areas. It is a pain-free treatment. Treatment is most effective in babies between 4-7 months and takes between 3-6 months to complete. Routinely babies up to the age of 14 months can be treated very successfully but treatment may take longer and results may not be as good with younger babies. To be effective, the device should be worn continuously (up to 23 hours a day).
- In cases of craniosynostosis, where the plates of your baby's skull have fused too early, surgery may be needed to move the bones.
We have designed a poster called Baby in Motion which focuses on helping to encourage development and tummy time in the early stages.
Coordination Difficulties
Developmental co-ordination disorder (DCD), also known as dyspraxia, is a condition affecting physical co-ordination that causes a child to perform less well than expected for their age in daily activities and appear to move clumsily. It is most commonly diagnosed around five years of age or older and has to be made by a Paediatrician.
It is thought that up to 1 in every 20 children between seven and eight years of age may be affected by the condition to some degree and present with a global coordination problem. DCD is thought to be around three or four times more common in boys than girls and the condition sometimes runs in families.
Although DCD does not affect how intelligent a child is, it can make it more difficult for them to learn and they may need extra help to keep up at school.
Signs/Difficulties?
In young children with DCD, early developmental milestones of rolling, crawling, walking, self-feeding and dressing may be delayed or slow.
Older children may have difficulties:
- with playground activities such as hopping, jumping, running, and catching or kicking a ball. They often avoid joining in sport activities because of their lack of co-ordination and may find Physical Education difficult. Some children with DCD may also become less fit than other children as their poor performance in sport may result in them being reluctant to exercise.
- walking up and down stairs
- writing, drawing and using scissors – their handwriting and drawings may appear scribbled and more childish than other children their age
- getting dressed, doing up buttons and tying shoelaces keeping still – they may swing or move their arms and legs a lot and find it hard to sit still.
- by appearing awkward and clumsy as they may bump into objects, drop things and fall over a lot.
Children with DCD can also have a range of other problems, such as:
- difficulty concentrating – they may have a poor attention span and find it difficult to focus on one thing for more than a few minutes
- difficulty following instructions and copying down information – they may do better at school in a one-to-one situation than in a group, as they are able to be guided through work
- being poor at organising themselves and getting things done
- not automatically picking up new skills and needing encouragement and repetition to help them learn
- difficulties making friends – they may avoid taking part in team games and may be bullied for being ‘different’ or clumsy
- behaviour problems – often stemming from a child’s frustration with their symptoms
- low-self esteem
Causes?
Little is known about the cause of developmental co-ordination disorder (DCD), although it is thought to be caused by a problem in the development of the brain. Performing smooth, planned movements is a complex process, involving your senses, muscles and central nervous system (brain, nerves and spinal cord). Any problem in this process could potentially lead to difficulties with movement and co-ordination.
There might be a link between DCD and:
- being born prematurely (before the 37th week of pregnancy)
- being born with a low birth weight
- having a family history of DCD, although it is not clear exactly which genes may be
- involved in the condition
- the mother drinking alcohol or taking illegal drugs while pregnant
Treatment?
There is no cure for DCD, but a number of therapies can make it easier for children to manage their problems. A small group of children, usually those with mild symptoms of clumsiness, may eventually ‘grow out’ of their symptoms. But the vast majority of children will need long-term help and will continue to be affected as teenagers and adults.
Treatment for DCD will be tailored to your child and usually involves a number of different healthcare professionals working together.
- Paediatric Occupational Therapy - assess your child’s abilities in daily activities, such as handling cutlery, dressing, using the toilet, playing and school skills involving fine movement activities (such as writing), as well as other aspects of how your child functions in the school and at home. The therapist can then work with your child, you as parents and teachers to help find ways to manage any problems.
- Paediatric Physiotherapist - assessing your child’s motor (movement) skills and abilities before devising an individualised therapy plan which may include activities to help improve walking, running, balance and co-ordination.
- Clinical Psychologist – a healthcare professional who specialises in the assessment and treatment of mental health conditions
- Educational Psychologist – a professional who assists children who are having trouble progressing with their education due to emotional, psychological or behavioural factors
At Children in Motion we will assess your child’s gross motor difficulties and devise a tailored Physiotherapy programme accordingly. In our experience this group of children require regular therapy input over a 1-2 year period to successfully address asymmetries, poor core muscle activity and limb girdle stability which help to improve balance and coordination difficulties.
Developmental Delay
What is Developmental Delay?
Developmental Delay on its own is not a diagnosis, but the term is used to describe a child's condition if they are not progressing as expected. All babies and children develop at different rates. Babies will learn to sit, crawl and walk at different ages but this may vary a lot. However, there are normal age ranges when most babies and children learn to do certain things, this forms a guideline for professionals. In some cases developmental delays may be diagnosed when there are problems such as:
- Movement and motor skills delay
- Speech and Language delays
- Visual problems
- Social and emotional skills delays/difficulties
- Thinking and cognitive skills delays
Sometimes, a delay occurs in many or all of these areas. When that happens, it is called "global developmental delay".
If a baby is not reaching their developmental milestones they may be referred for an assessment with a Paediatrician and a Child Development Team. They may then be referred for specific help such as Physiotherapy, Occupational Therapy and Speech and Language Therapy.
Sometimes a child that shows some delayed development will be able to catch up with the right help.
Sometimes their development may be slower than other children because they have underlying learning difficulties or more rarely other underlying health conditions. Very rarely, a child may lose skills that they have learnt and their development starts to slow or go backwards.
If you are worried about your child's development the best person to speak to is your GP or Health Visitor. They can decide whether a child needs to be referred to the Child Development Team. Unfortunately in many cases these processes can take a long time and a problem that could have been sorted out with early intervention then becomes a bigger issue that requires longer term intervention. Therefore if you have any concerns about your baby’s development contact a Physiotherapist who specialises in the treatment of children for an assessment as soon as possible. Some areas in the UK offer a self-referral service, which means you can make an appointment to see a NHS Physiotherapist without having to see your GP first.
At Children in Motion we are highly experienced in child development problems and early intervention. Where possible we aim to see your baby within a week if possible to do a thorough assessment. Following the assessment we will discuss with you whether we think Physiotherapy alone would be enough or whether your child needs to be referred to a Paediatrician and/or other health care professionals.
Torticollis
Torticollis is a term used to describe the baby’s head being held tilted to one side and the face turned to look towards the other side. It is due to tightness of the muscle on one side of the neck. The cause of muscle tightness is often uncertain but may be related to the position the baby was in the womb.
The baby may continue to keep their head looking in one direction. There will often be plagiocephaly (flattening on the back of the head), on the same side, with restriction of head movement in the opposite direction. Torticollis usually improves without any long-term effects, but may impact on a baby’s gross motor development.
At Children in Motion input is aimed at positioning advice, reducing the tightness in the neck, facilitating the development of optimal movement patterns and reducing asymmetrical habitual patterns. After the torticollis has been resolved a baby is often seen on a review basis to ensure that the asymmetrical habitual patterns do not recur and that their development continues to progress as expected.
Syndromes
There are many different types of syndromes of which Down’s Syndrome is probably the most common and well known.
Although different types of syndromes differ in their symptoms, a lot of syndromes have hypotonia (low muscle tone/floppiness) as one of their main problems. Depending on the severity of the low muscle tone it may lead to gross motor developmental delay and joint laxity (joint hypermobility). They often find ways to compensate for the differences in their physical make-up, and some of the movement compensations can lead to long-term complications, such as pain in the feet or the development of an inefficient walking pattern.
At Children in Motion we aim for these children not to necessarily accelerate in the rate of their development, as is often presumed, but to facilitate the development of optimal movement patterns and therefore improve the quality of their movement. This means that over the long term, we want to help the child develop good posture, proper foot alignment, an efficient walking pattern, and a good physical foundation for exercise throughout life.
Flat Feet
Most normal feet have an arch along the inside length of the foot. A flat foot is when this arch seems absent or reduced when your child is standing. There are many bones in the feet, which are held together by ligaments. Flat feet are usually due to lax or loose ligaments. This causes the arch to flatten when your child stands up. Flat feet can also be caused by tight muscles and turning in of the hips.
Between 3 and 13% of children have flat feet and the condition is more common in younger children. Before the age of 3 all children have flat feet, as the arch on the inside of the foot does not begin to develop until after this age. It can be normal for a child to be slightly flat footed until eight to nine years old. Being flat footed does not necessarily cause any problems, but it is important that it is assessed by an experienced children’s Physiotherapist to see what the cause is and if treatment is needed.
The typically flat-footed child has what's known as a flexible flat foot, where the arch is present but disappears when the foot bears weight. When this is associated with symptoms such as foot, ankle or knee pain, poor balance, poor stamina in walking or disability, Physiotherapy treatment should be offered.
Treatment?
Physiotherapy – a thorough assessment should be carried out by an experienced children’s Physiotherapist followed by advice and/or active treatment including stretches and strengthening exercises.
Orthotics – your child may be referred to an Orthotist or Podiatrist for customised insoles which will help to correct the arches of the foot when wearing ordinary shoes. This will help to reduce the negative impact of a poor foot posture on the rest of the body.
Simple footwear advice such as a well-fitted, supportive shoe with built-in arch support can help.
If your child does not have any associated problems with their flat feet it may be that they do not need any intervention. On the other hand, children without symptoms need monitoring over time.
At Children in Motion we feel it is very important to look at the child holistically and not just at the foot in isolation. We therefore do a thorough assessment of the whole body and a functional movement analyses to ensure there aren’t any hidden causes, compensations or knock-on effects elsewhere that needs addressing.
Unknown
It could be that your child has a developmental delay or physical disability, but that you are still in the process of receiving a diagnosis or that your medical team is not able to pinpoint the actual cause at all.
From a Physiotherapy point of view this does not stop us or delay therapeutic intervention as we mainly 'treat what we see'. If you are in this very difficult position please contact us to see how we can help your child.









































 Facebook
Facebook Instagram
Instagram